Pancreaticoduodenectomy
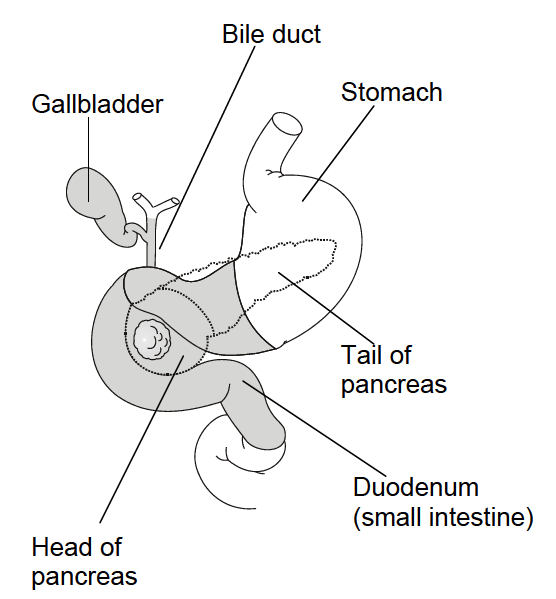
Panctreaticoduodenectomy (PD) is most commonly performed for pancreatic head and periampullary malignancy, but may also be indicated in select cases of chronic pancreatitis or benign periampullary tumors. It is a major operation that involves the removal of the head of the pancreas, the duodenum, the gallbladder and the common bile duct (Figure 1). A short length of small intestine beyond the duodenum is also removed. In the classic Kausch-Whipple operation, the pylorus (outlet of the stomach) and the distal (lower) part of the stomach are removed, while in the Longmire-Traverso operation (pylorus-preserving pancreaticoduodenectomy), the stomach and the pylorus are not removed.
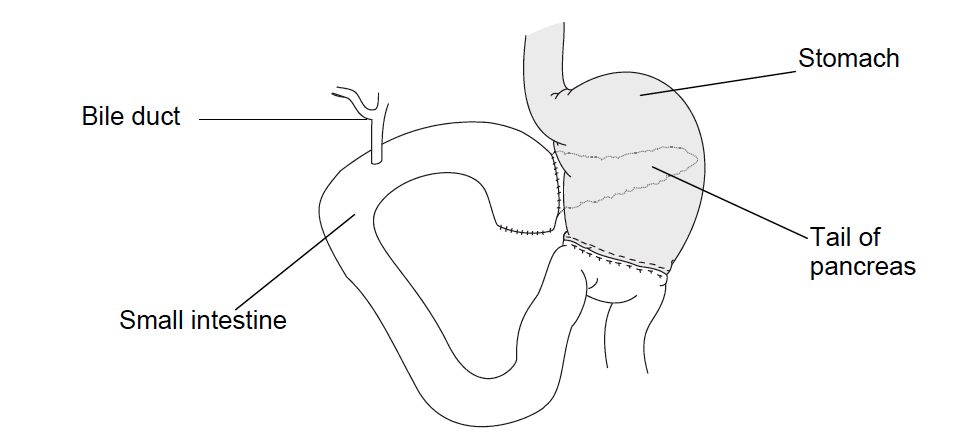
After resection, the end of the remaining bile duct; the remaining pancreas and the stomach are then connected to the small bowel to ensure flow of bile, digestive juices and food into the intestines (Figure 2). Three anastomoses are constructed:
- Pancreatic anastomosis. The pancreatic remnant is anastomosed to the jejunum (pancreatico-jejunostomy) or to the posterior wall of the stomach (pancreatico-gastrostomy).
- Biliary anastomosis. Hepatico-jejunostomy is performed between common hepatic duct remnant and a site on the jejunum distal to the pancreaticojejunal anastomosis.
- Enteric anastomosis. In Whipple PD, an antecolic anastomosis is constructed between the stomach and the jejunum; in Longmire-Traverso PD, an antecolic duodeno-jejunal anastomosis is created.
Different technical modifications of reconstruction techniques have been proposed, but none resulted superior in meta-analyses. The choice of the reconstruction technique to adopt depends on the surgeon’s preference and institutional practices.