Pancreatic cystic neoplasms – Overview
Although considered uncommon, cystic neoplasms of the pancreas have been increasingly diagnosed due to the widespread use of cross-sectional imaging. In fact, in tertiary care centers with experience in pancreatic surgery, the proportion of pancreatic resections carried out for cystic neoplasms has doubled in the last two decades; in parallel, the number of patients enrolled in surveillance protocols has dramatically increased.
Pancreatic cystic neoplasms encompass a broad spectrum of benign, malignant, and borderline lesions. Many aspects of their biological behavior have been recently clarified, although an understanding of the natural history of mucinous forms – and especially of branch-duct intraductal papillary mucinous neoplasms – is limited by the difficulty of distinguishing accurately between benign, malignant, and potentially malignant lesions before surgical resection. Furthermore, current guidelines for the management of pancreatic cystic neoplasms are based on the assumption that these lesions can be classified correctly on the basis of their cross-sectional imaging features. However, there is a certain degree of morphological overlap between different lesions such that the possibility of an inaccurate preoperative characterization must always be taken into account. The diagnosis of pancreatic cystic neoplasms requires both a familiarity with the morphological spectrum of these lesions and the collaboration between surgeons, radiologists, gastroenterologists and pathologists, to increase the likelihood of appropriate management. Yet, some aspects of the management of pancreatic cystic neoplasms remain unclear, and, especially for mucinous neoplasms, the clinical and radiological work-up is not always able to predict the likelihood of progression to invasive cancer in a given patient.
This has generated controversies as to whether patients should be offered resection or, alternatively, enrolled in surveillance protocols with periodic imaging. This is a relevant issue because these neoplasms are mostly diagnosed in asymptomatic patients who underwent cross-sectional imaging for unrelated problems. Among the many other unsettled aspects are the appropriate timeframe for surveillance, the role of cyst-fluid analysis and cytology, the role of atypical resections and of lymphadenectomy, and the recurrence rate of IPMNs and their association with other non-pancreatic neoplasms.
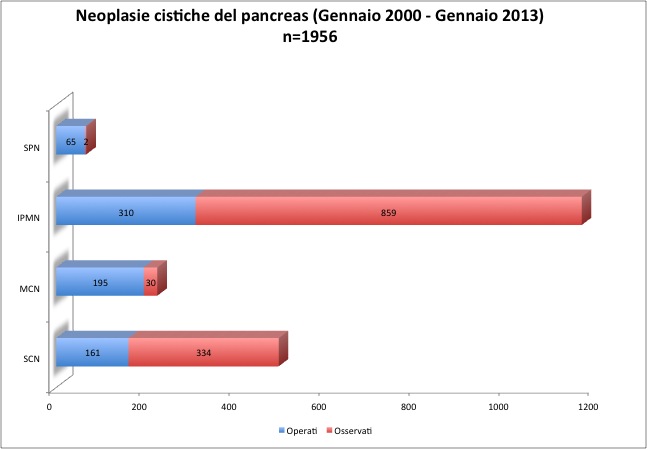
At our institution, more than 1900 patients with pancreatic cystic neoplasms presented between 2000 and 2012. Figure 1 shows our pancreatic cystic neoplasm caseload, divided by cyst type and management.