radiofrequency ablation of locally advanced PDAC
Radiofrequency ablation of pancreatic neoplasms is an experimental technique that has been deveoped by a research consortium (Unit of Pancreatic Surgery at the Peschiera del Garda Hospital and Unit of Pancreatic Surgery in Verona). It is currently employed in patients with locally advanced ductal adenocarcinoma (PDAC).
Radiofrequency ablation (RFA) is a local ablative method that can destroy the tumour by thermal coagulation and protein denaturation. RFA has been used successfully in the treatment of unresectable solid tumours in the liver, lung, kidney, brain, breast, prostate, bone, adrenal glands and spleen. Application of RFA to the pancreas presents potential problems related to the properties of the pancreatic parenchyma (soft and friable) and to the risk of inadvertent thermal injury to the distal common bile duct, duodenum, transverse colon and portal vein.
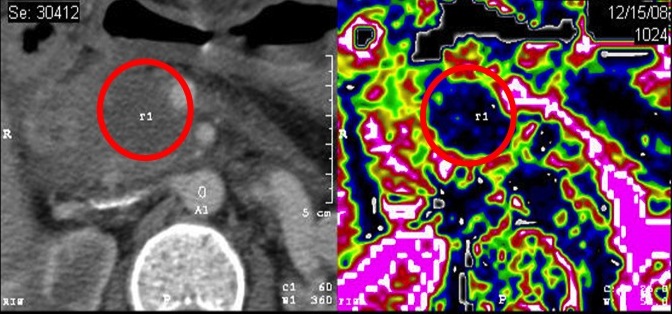
Our group demonstrated in 2010 the feasibility and safety of pancreatic radiofrequency ablation in a group of 50 patients. Mortality was 2% and morbidity was 24%. Furhter technical refinements have been applied, such that mortality has decreased to 1%, and the severity profile of complications has substantially improved. To date, we have performed more than 200 procedures, and we are investigating the role of radiofrequency ablation in the context of a randomized clinical trial. Figure 1 shows the effects of radiofrequency ablation of a locally advanced pancreatic head ductal adenocarcinoma as seen on postoperative perfusion-CT scan.
Radiofrequency is a palliative procedure, the presence of residual viable tumor at the periphery of the treated area being an intrinsic aspect of the procedure. Survival data of patients treated in Verona, calculated from an observational non-randomized analysis, seem encouraging. Radiofrequency ablation seems to be a locally effective approach, and may be considered as part of a multimodal treatment for advanced pancreatic ductal adenocarcinoma. Current indications to radiofrequency include:
- Confirmed locally advanced pancreatic ductal adenocarcinoma (radiologic staging + biopsy)
- Age 18-80 years
- Stable or locally progressive disease after chemotherapy or chemoradiotherapy
- Performance status >50% (Karnofsky) or <=2 (ECOG)
Radiofrequency ablation is performed via a laparotomy. Accurate exploration of the peritoneal cavity is performed and supported by intraoperative ultrasonography in order to rule out previously undetected metastases and confirm unresectability of the lesion. The probe is placed in the centre of the lesion under ultrasonographic guidance, intraoperative ultrasonography is also used during the procedure to monitor the coagulative effect. When technically feasible, a biliary and gastric bypass is performed in patients with tumors of the pancreatic head. Gastric bypass is performed only if necessary in patients with tumors of the body-tail.
Raiofrequency ablation is a major surgical procedure to be carried our in centers with broad experience in pancreatic surgery. A careful multidisciplinary evaluation (surgeon, radiologist, oncologist) is necessary to design the best care plan for each patient.
Although in expert hands radiofrequency ablation is safe, post-operative morbidity (similarly to pancreatic resections) is substantial. Postoperative complications associated with radiofrequency ablation of pancreatic solid tumors include:
- Portal vein/superior mesenteric vein thrombosis
- Ischemic duodenal ulcers
- Thermal acute pancreatitis
- Pancreatic fistula and abdominal collections
CT-scans are performed after 7 and 30 days from the procedure to monitor the ablated area. The patients are referred to the Oncologist for possible prosectution of chemotherapy or chemo-radiotherapy, and are enrolled in a strict surveillance protocol, including a detailed clinical examination, measurement of serum Ca 19.9, and cross-sectional imaging.
Learn more:
Girelli R, et al. Br J Surg. 2010;97:220-225.
Cantore M, et al. Br J Surg. 2012;99:1083-1088.